COVID-19 poses extraordinary challenges for experiential, outdoor, travel, and adventure programs. But understanding best practices can help organizations successfully navigate the pandemic.
[This article originally appeared on OutdoorEd.com: The Premiere Community for Outdoor Education Professionals. ]
Introduction
COVID-19 represents a crisis and global tragedy in many ways. Yet there are clear pathways for outdoor and other experiential programs to continue to achieve their mission, despite the pandemic.
We’ll cover general principles for sustaining organizations in the face of the disease, best medical practices for preventing and mitigating effects of virus transmission, and systems-informed responses to the pandemic.
General Principles
An outbreak of a novel virus first encountered in December 2019 led to an epidemic and then a pandemic, and within six months the disease killed almost a million people, a tragic milestone it soon surpassed, marking COVID-19 as a global catastrophe of historic proportions.
The pandemic has dramatically changed how billions of people across the planet live, work, and seek to maintain safety for themselves and others—and outdoor programs, too, have been drastically affected.

Note: best practices are changing rapidly. The response to the pandemic continues to evolve. What is emerging as best practice now may change quickly. So stay alert for new information, and recognize that the ideas presented here may become outdated rapidly.
The severity of the pandemic and responses to COVID-19 vary widely between regions, due to a variety of factors.
However, we can ascertain certain general principles with wide applicability to outdoor programs globally. These are to:
- Follow guidance from public health agencies
- Pay attention to information from outdoor industry associations
- Work cooperatively with other outdoor programs
- Address the pandemic with the seriousness it deserves, and
- Hold strong in the face of this monumental challenge
Let’s look at each of these five principles in detail.
Follow Public Health Guidance
First, it’s critical to carefully follow the recommendations and requirements of public health agencies. This includes local health departments (for example, at the city or county level) and sub-national agencies (at the state, province, canton, or territory level). It also includes national Centers for Disease Control or the equivalent, and the World Health Organization.
In addition, other governmental entities may have important health and safety guidance. These may include departments of commerce, labor, or industry, which regulate business and commercial activity, for example restricting certain business activities and issuing requirements for employee health.
It may include childcare regulatory entities that address child safety at youth camps or elsewhere.
And it may include central government departments addressing international travel, such as a Foreign Affairs ministry or Department of State.
Public health guidance based on sound science is reputable, but recognize that even capable health agencies can be negatively influenced by political factors, so use good judgment and understand that in rare cases, exceeding the recommendations issued by authorities may be appropriate.
It’s useful to pay attention to broadly applicable health guidance, like mask-wearing and social distancing, but also to follow outdoor programs-specific recommendations disseminated by public health entities, when available.
For instance, the US Centers for Disease Control and Prevention provides detailed expert guidance on safety measures for youth programs and camps (https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/summer-camps.html), as well as other types of activities (https://www.cdc.gov/coronavirus).

Public health authorities in Queensland Australia require businesses to have an approved COVID Safe Industry Plan. The government provides comprehensive plan templates and checklists specifically developed for outdoor education providers, and outdoor recreation providers, and others (covid19.qld.gov.au/government-actions/approved-industry-covid-safe-plans).
Use Industry Association Resources
Second, it’s useful to take advantage of guidance developed or compiled by your relevant outdoor industry association or trade group.
The American Camp Association, for example, commissioned an extensive, eighty-seven page report on how camps can apply public health guidance to their particular context (https://www.acacamps.org/resource-library/coronavirus-information-camps).
Numerous other industry groups have assembled or prepared information specific to the needs of their members. A partial list of examples includes:
- Association of Outdoor Recreation & Education https://aore.org/coronavirus.php
- AEE https://www.aee.org/community-resource-library
- The Alliance Collaborative, https://thealliancecollaborative.com/covid-19-resources/
- Climbing Wall Association https://climbingwallindustry.org/page/Coronavirus
- Association for Challenge Course Technology https://www.acctinfo.org/page/coronavirus
- National Recreation & Park Association https://www.nrpa.org/our-work/Three-Pillars/health-wellness/coronavirus-disease-2019/
- Outdoor Play Canada https://www.outdoorplaycanada.ca
- North American Association for Environmental Education https://naaee.org/eepro/resources/eeguidance-reopening-schools
- Adventure Travel Trade Association https://www.adventuretravelnews.com/covid-19-guide-for-the-adventure-travel-industry
- World Travel & Tourism Council https://wttc.org/COVID-19
- Overseas Security Advisory Council (OSAC) Academia Working Group (education abroad) https://www.osac.gov
- Event Safety Alliance https://www.eventsafetyalliance.org
- International Association of Amusement Parks and Attractions https://www.iaapa.org/news/covid-19-resource-page
Connect with other Outdoor Professionals
Third, many program managers have found sound guidance and moral support in connecting with others navigating through the pandemic, sharing information on what works and what doesn’t, and offering encouragement in a challenging time.
Avoid Underestimating the Situation
It’s important to be clear-minded about the seriousness of the pandemic. Some countries, such as New Zealand, Iceland, and Taiwan (as pictured below, with outdoor programs running in summer 2020), have managed the pandemic well and outdoor programs are back to near normal operation, where operations in other countries still face debilitating restrictions.

In regions where COVID-19 is not contained, outdoor programs are wise to recognize the extraordinary business continuity challenges present, and the absence of obvious solutions. This means that adaptive organizations are psychologically and operationally open to re-inventing from the ground up how they meet the organization’s mission, and embrace rather than avoid the imperative to change.
This involves avoiding cognitive biases such as ‘normalcy bias,’ the tendency to fail to prepare for a rare but serious incident, and fail to adequately respond if it occurs—essentially, a form of denial of reality.
Examples of how experiential and outdoor programs have made dramatic and creative shifts in program delivery include the JUMP! Foundation’s rapid shift from in-person to online team-building programs, and the major transition of Outdoor Adventures by Boojum’s delivery model from large school-group backpacking and other outdoor trips to offering a wifi-enabled space for school students to do class work remotely along with occasional socially distanced in-person teambuilding games.

Embracing creative responses can mean finding brand-new methods for achieving the same programmatic outcomes, such as building life skills and team skills in a local park rather than on a travel-intensive trip where distancing is inherently challenging. And activities like high ropes challenge courses with high perceived risk can have powerful impacts when courses are configured for distanced operation.
Because experts say the virus may be with us for years, outdoor programs might consider investing in longer-term changes, like re-modeling sleeping accommodations for enhanced support of distancing and hygiene, making indefinite work-at-home arrangements, and the like.
For communities in which the virus is not contained, leaders may expect to encounter uncertainty and the need for creative problem-solving to generate their own solutions that work for their situation.
Hang In There
And fifth and finally, hang in there! These are challenging times we are all living though, but you’re not alone. We will overcome this pandemic, together, and the tenacity and team effort you bring forward can help lead to a successful outcome for your outdoor program and beyond.

Best Medical Practices
COVID-19 has dramatically affected outdoor programs, and understanding best medical practices is essential for managing the pandemic.
Responses to the disease are evolving, but best medical practices for outdoor programs are sufficiently well-established to provide powerful and effective guidance.
We’ll approach this medical guidance as it applies to each of the eight direct risk domains, or risk reservoirs, where risks reside: culture, activities and program areas, staff, equipment, participants, subcontractors, transportation and business administration.
Introductory Concepts
But before we go into detail in each risk domain, let’s address seven introductory concepts to frame this conversation.
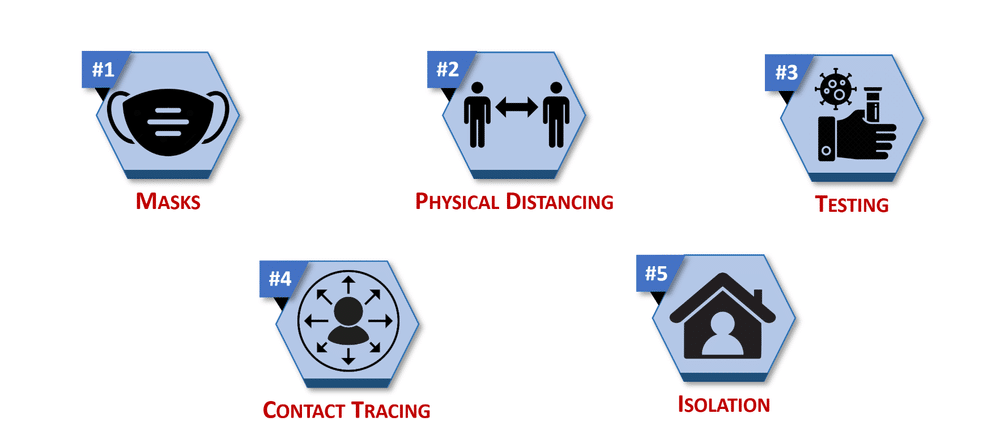
First, the remarkable fact that if five basic, well-established public health practices—mask use, physical—or “social”—distancing, virus testing, contact tracing and isolation and quarantine—were followed, globally, the COVID-19 pandemic could be brought under control in weeks (youtu.be/jzHIhSZ_fiA?t=318). This could have happened in spring of 2020 in the earliest stages of the pandemic.
Following these practices might eliminate entirely the need for a vaccine.
But these practices come with major short-term economic, social and political costs, and, needless to say, have not been uniformly implemented.
Second, there’s no one single thing that will halt the march of the disease; rather, an effective response demands appropriately using many public health tools.
The focus should be on doing enough of the right things, correctly. If all the recommended public health procedures, adapted for your context, are followed, disease transmission is preventable. But if even one element—like hygiene, screening, distancing, mask use, or an appropriate safety culture—is missing, then the whole effort may collapse.
Third, this means that if we selectively employ only a partial set of interventions, we dramatically increase the probability of disaster, as we’ll see shortly in two case studies.
Fourth, which measures should be taken and how varies according to the severity of the pandemic in the local area.
Fifth, adjustments should be made for very young children and others needing extra support, for example, those who cannot remove a mask without help or safety use hand sanitizer unsupervised.
Sixth, anticipate the need to accommodate conflicting guidance from various entities, for example with an itinerary that traverses areas managed by different governmental bodies or land managers.

Finally, since the information here is drawn in part from the US CDC’s guidance for youth programs and camps, modifications may be necessary for your unique situation. Regularly and closely consult your applicable public health agencies for detailed guidance for your specific circumstances.
Culture
We’ll begin with culture, which refers to the underlying beliefs and values that drive behavior.
Fostering the beliefs, values, knowledge and skills in support of good public health measures is critical for helping ensure those practices are followed.
The appropriate training, supervision, signs and other procedures and messaging are necessary to support that positive safety culture.
Activities and Program Areas
Changes to activities and programs areas are a major focus. Limiting sharing between people is a key element here. This can include closing group spaces like dining halls, or restricting use to small groups and disinfecting between uses.
Replacing high-touch items like bulk snacks with single-serve items can be useful. Prohibiting shared use of personal or group items unless they’re disinfected is also a best practice.
Restricting visitors, observers, and contact with anyone outside a small group cohort is important as well.
Options for pandemic-informed food service include having participants bring own meals, eat in small groups, use disposable food service items, use pre-packaged food instead of buffet or family-style meals, and avoid sharing food or utensils.
Significant changes to program activities can substantially reduce risk.
A number of outdoor programs have found success in taking previously hands-on outdoor experiences completely virtual.
For example, the Breckenridge Outdoor Education Center invites participants on guided virtual hikes, and suggests follow-up activities like taking a hike of their own, identifying wildflowers, and sharing pictures of their outdoor adventure online.

Other organizations have replaced multi-day expeditions with single-day and other short programs, which make physical distancing easier.
Summer camps are opening as spaces for remote learning, where students log in to their online school classes in an attractive camp setting better set up for distancing than an urban living situation.
Sports-type activities with heavy breathing and close contact, such as basketball, are being replaced with distancing-friendly alternatives (such as tennis and some swimming setups).
Backcountry, front-country or urban expedition routes are being adjusted to avoid potentially congested areas.
Staff
Practices for protecting employees and other staff include re-writing personnel policies to establish when it’s safe to return to work after an infection, establishing back-up personnel in case staff get sick, building in structures such as remote work, flexible leave options, and modified job responsibilities to limit virus exposure, and appointing a visible lead to oversee pandemic response and communication.
And organizations can reinforce the capacity of staff’s immune systems to fight off infection by encouraging alternatives to over-consumption of distressing news reports, and supporting appropriate diet, exercise, sleep, relaxation time, and access to emotional support and counseling.
Equipment
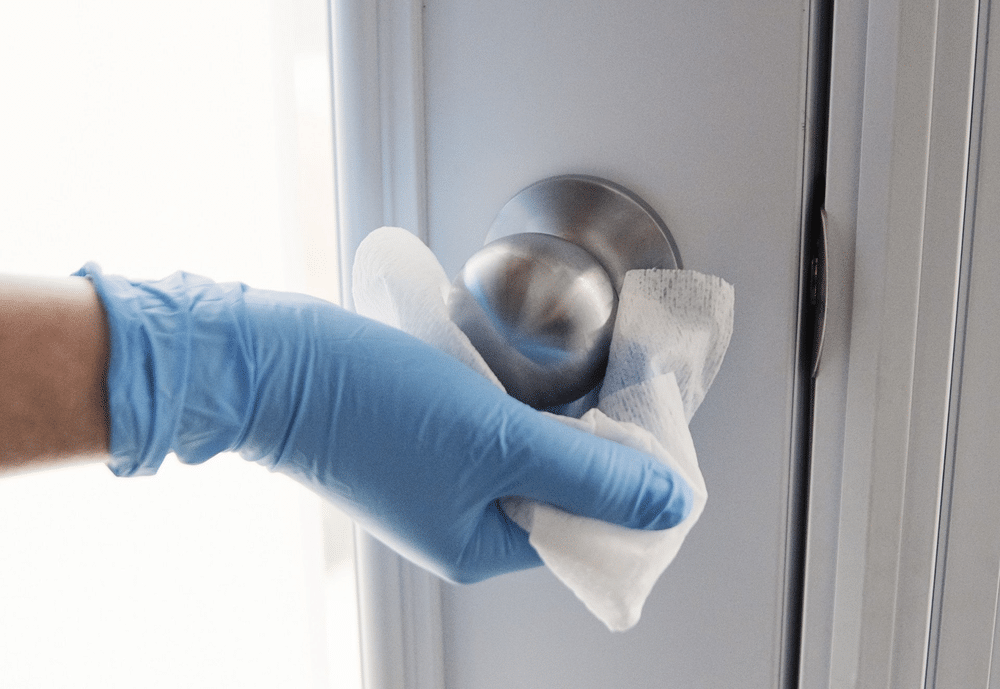
Risk of infection from equipment, which includes outdoor gear and supplies, vehicles, and buildings and their contents, can be reduced by frequently cleaning and disinfecting high-contact items and surfaces like door handles, railings, tables and desks.
Areas used by sick persons should be closed off for 24 hours then disinfected, before they are re-used.
Consult your health or environmental agency for a list of approved disinfectants. An example list applicable in the USA is available at https://www.epa.gov/pesticide-registration/list-n-disinfectants-coronavirus-covid-19.
Adequate cleaning and disinfecting supplies, including personal protective equipment, must also be kept available.
Since research now indicates the SARS-CoV-2 virus may linger in the air for hours, posing an aerosol, or airborne, transmission risk far beyond two meters, especially in indoor spaces with poor ventilation, and in places where people talk loudly or sing, group activities should preferentially take place outdoors.
Indoor spaces should be well-ventilated, for example by opening doors and windows and using fans, and high-efficiency air filters should be used in ventilation systems when feasible.
Facilities managers should consult ventilation industry guidance (such as provided by such as ASHRAE, the American Society of Heating, Refrigerating and Air-Conditioning Engineers, www.ashrae.org/technical-resources/resources) for further resources on specific topics such as re-opening buildings and use of UV light as a disinfectant.
Physical barriers like sneeze guards and partitions should be installed as appropriate. Physical guides like markers indicating one-way foot traffic and how far apart to stand from others while waiting in line are also helpful.
Participants
Our fifth risk domain is Participants. (Procedures here also apply to select staff, such as those working directly with participants.)
Cohorting, or dividing groups of participants and associated staff into small groups, or bubbles, which stay apart from each other, is an essential tool for minimizing transmission risks.
Cohorts can stagger use of communal items and spaces like dining halls to prevent cross-cohort interaction. If an individual in a small group cohort becomes symptomatic, they are isolated and tested while the remainder of the cohort is quarantined from others, but may continue outdoor programming as a cohort.
The need for physical distancing outside of households is also well-established, at a distance of at least six feet or approximately two meters or following health agency guidelines. Note that coughing and sneezing can propel droplets more than six meters (20 feet).
Plastic or other impermeable barriers can be installed between desks or between service workers and customers.
Exposure times should be minimized: shorter contact is better.
On overnight programs, individuals in bunk beds should sleep head-to-toe (as pictured), or use one-person tents or tarps.

Close contact with passers-by should be avoided.
It’s essential to wash hands frequently with soap and water (either warm or cold; both are acceptable) for at least twenty seconds. If soap and water are not available, hand sanitizer with at least sixty percent alcohol should be used. Coughs and sneezes should be covered with a tissue, mask, or elbow. Tissues should be discarded after use, and hands should then be washed.
Appropriate mask use is also essential. Good mask use may be more effective than a vaccine, according to the director of the U.S. Centers for Disease Control and Prevention (youtu.be/NhV0vtkkchc?t=24).
Masks should be plentifully stocked in first aid kits and elsewhere. N95 masks without exhalation ports and surgical masks are best, but should be reserved for health workers unless supplies are abundant. Cloth masks don’t protect wearers well but stop some particles. And face shields are typically ineffective alone, but can be used in addition to masks.
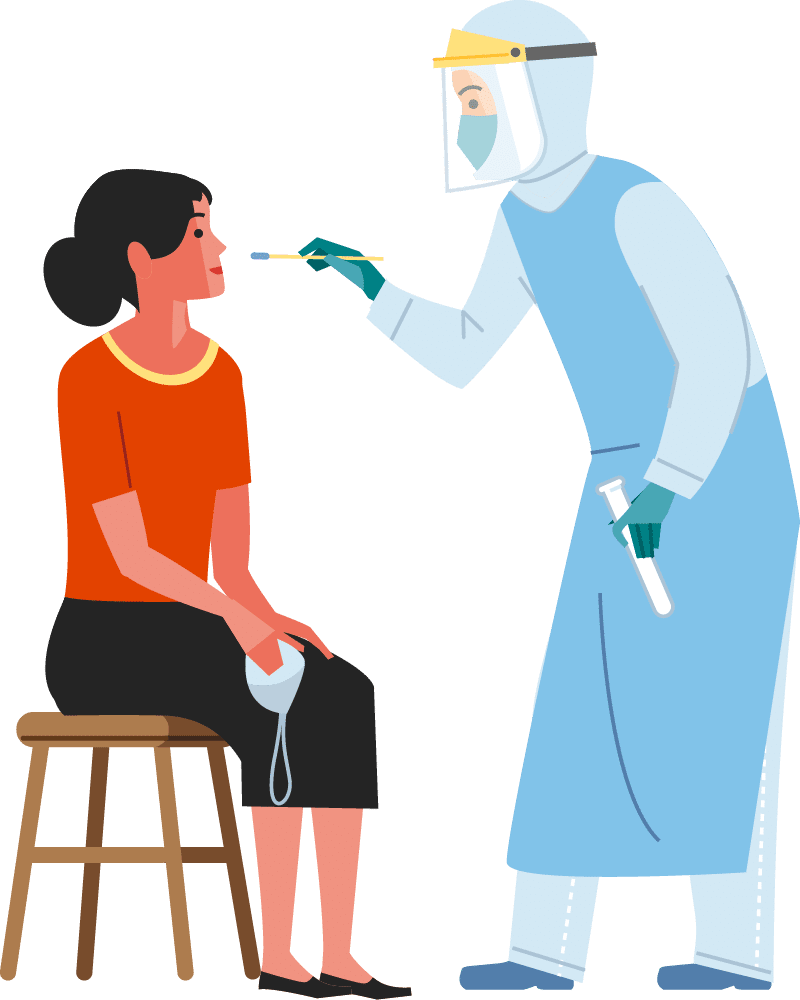
Medical screening for COVID-19 starts by staying home if you’re sick, test positive, show COVID-19 symptoms, or recently had close contact with a person with COVID-19.
However, since approximately 40 percent or more of those infected show no symptoms, measures like mask use and distancing must still be used.
Persons showing symptoms should receive rapid testing and be isolated from others, with contact tracing if test results are positive, with quarantine of those contacts.
If the test is negative, isolation can end following a waiting period of a duration established by the local health agency.
Note that some of these procedures, like symptom screening and isolation, are generally well in control of the outdoor program. Others, such as testing and contact tracing, are often in large part controlled by health authorities. Effective participation from both parties is necessary for good virus control.
Outdoor programs should conduct frequent symptom checks of participants and associated staff, for example every day.
Symptoms may appear 2-14 days after exposure to the virus. People with these symptoms may have COVID-19:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Frequent COVID-19 testing is also appropriate, using viral or antibody tests, following health agency guidance (https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/testing.html).
The outdoor program should employ isolation protocols for symptomatic persons, and quarantine procedures for those who may have contacted the symptomatic person, following health agency guidelines. Arrangements for transportation of these persons should be developed in advance.
Protocols to safeguard higher-risk individuals should be in place. For example, older or immunocompromised individuals should avoid interaction with participants, gear, or program areas.
Place-based programs such as a summer camp can select participants from the local geographical area to limit risks of carrying or encountering viruses through travel.
Subcontractors
Subcontractors and outside users of a program’s facilities (such as facility renters) should be required to follow appropriate safety procedures.

Transportation
In our next to last risk domain of Transportation, procedures should be developed and implemented to reduce transmission risks in transportation to, during and from the program, including in both normal program operations and medical evacuations.
Changing which program areas are used, and how they’re used, should be considered, in order to structurally reduce the need for transportation at all.

Business Administration
In our final risk domain of Business Administration, outdoor programs should adjust their communications strategy in light of COVID-19.
This involves re-designing written and other communications to ensure that informed consent to the risks of COVID-19 is appropriately provided.
It also involves ensuring that detailed protocols are in place for two-way communications with the health department, staff, participants, and family members or guardians of participants in case of actual or suspected infection.
Conclusion
This is a summary only of best medical practices for outdoor program management of COVID-19. Standards may change rapidly, so consult local, regional, and national public health entities for additional important details and up-to-the-minute guidance.
Systems-informed Response
Let’s conclude our discussion of COVID-19 impacts on outdoor program risk management by looking at systems-informed responses to the pandemic.
We’ve previously addressed general principles and best medical practices. Now, systems-informed responses we’ll cover include considerations of insurance coverage, legal liability, implications of vaccines, re-opening businesses, underlying causes of pandemics, and readiness for future disruptions.
Insurance
Insurance policy coverage of the COVID-19 pandemic is in some cases unsettled; it’s wise to check your policy language and discuss possible exclusions with your agent.
Examples of relevant insurance include, but are not limited to, liability, medical, international evacuation/repatriation, business interruption, Directors & Officers, unemployment, and worker’s compensation insurance.
Legal proceedings may determine coverage when disputes arise, and policies clearly covering COVID-19 may become more widely available as insurers further develop pricing models and products.
Liability
Who pays for what if an employee or participant believes they’ve contracted COVID-19 at your organization? This is a legal topic that will become more settled over time, and as case law emerges from court cases in the jurisdictions applicable to your organization.
In order to manage liability issues, it’s important to revise language in forms signed by participants regarding acknowledgement and assumption of risk, release of liability, hold harmless, and indemnification, to address COVID-19, and to ensure prospective participants are informed of virus-related risks, and—well in advance of the program—voluntarily provide informed consent to being exposed to those risks.

Cancellation and refund policies may need to be adjusted, and you may consider requesting documentation evidencing completion of any required quarantine and/or isolation period prior to program participation.
Consult with a qualified attorney familiar with your program and legal aspects of COVID-19 to understand your legal responsibilities for disease prevention and response, and steps to take to manage liability if transmission on your program is suspected.
Vaccine

Vaccines are an important part of protection from viruses, but it’s worth noting that vaccines would not be necessary if standard public health practices were fully followed.
Since it may take years for a comprehensive global vaccination campaign with an effective vaccine to be completed, and because a vaccine may not effectively work in all persons or provide long-lasting protection (such as with the vaccine against the flu virus), a long-term need for physical distancing and other non-pharmaceutical measures may remain.
Re-Opening
When can a business completely or partially closed by the pandemic resume operations?
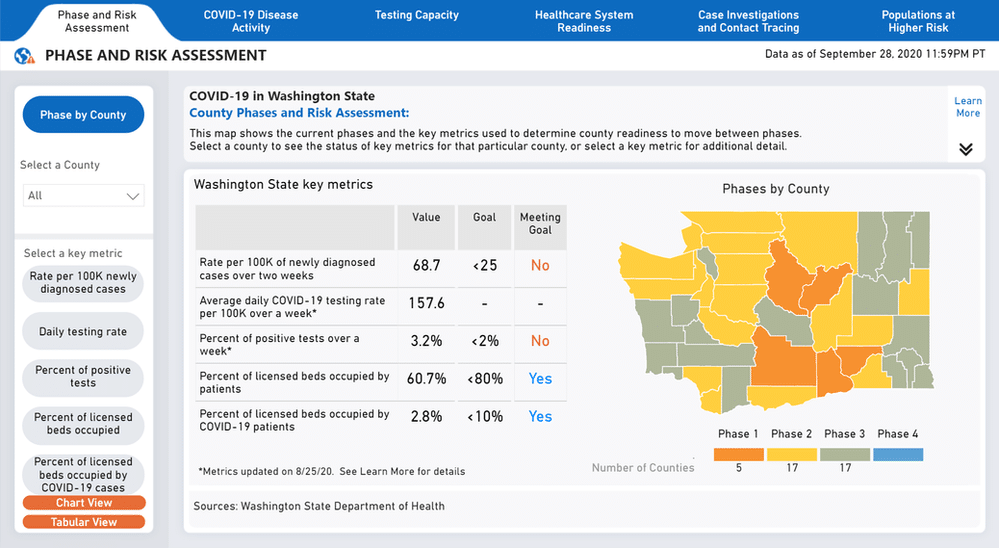
This judgment is typically made by local or regional government authorities, after consultation with public health agencies. Criteria vary but may include:
- The health care system has capacity to absorb new cases
- The rate of new cases/hospitalizations flat or decreasing
- Adequate testing and contact tracing capacity exist
- The business is capable of following medical best practices
Case Study 1
Let’s now take a look at some outdoor programs, steps they took to deal with COVID-19, and the measure of success they enjoyed.
The first case is a set of four summer camps in northeastern USA in the summer of 2020, with over a thousand attendees from seven countries. Using the standard public health approaches we’ve discussed, the camps provided a complete summer camp experience while successfully preventing and mitigating SARS-CoV-2 transmission.
The camps used a full battery of strategies, including
- Prearrival quarantine
- Pre- and post-arrival testing and symptom screening
- Cohorting
- Use of face coverings
- Physical distancing (between cohorts)
- Enhanced hygiene measures
- Cleaning and disinfecting
- Maximal outdoor programming
Before coming to camp, participants were quarantined with family members (unless parents were essential workers, in which case interaction with the camper was requested to be limited). Several days prior to arrival, campers were tested. If a prospective attendee showed symptoms, they were isolated for 10 to 14 days before arrival.

Transportation to camp was managed to reduce risks. Participants were encouraged to travel to camp using a private family vehicle if possible. On the camp bus, face coverings and physical distancing were employed. Attendees were instructed to use face coverings when on an airplane.
On arrival, attendees were divided into cohorts (bubbles), and quarantined by cohort for 14 days. Attendees stayed in their cohorts.
At camp, attendees were instructed in good hygiene, including cough & sneeze etiquette, handwashing, and use of hand sanitizer. Staff member were not permitted to leave camp on days off. Attendees were screened daily for COVID-19 symptoms.
Testing was conducted four to nine days after arrival. If a person tested positive or had symptoms, they were isolated, and their cohort was quarantined, until the attendee received negative test results. Serial (multiple) testing was seen as an important element in transmission prevention and mitigation.
Numerous program changes were instituted, including:
- Limit indoor activities that mix cohorts
- Stagger dining periods or dine outdoors
- Cohort-specific programming
- Bathrooms disinfected twice daily
- Cohorts based on living quarters
- Kitchens: state COVID-19 restaurant protocols followed
- Limiting sports to social-distancing-allowing ones
- If interacting outside the cohort: masks, distancing for 14 days
- Bathroom use cohorted, with separate bathrooms or staggered use
- Cleaning & disinfection per health agency guidelines
- Disinfect certain items after use, or wait 24 hours
- Single-use items like milk cartons, condiment packs, silverware
- Staggered meal times; buffets rather than family style
Out of 1022 attendees, three received positive test results after arriving, asymptomatic, at camp. Additional testing returned no positive results. No cohort members tested positively, and no secondary transmission was identified.

This remarkable feat of successful outdoor programming in the midst of a pandemic raging uncontained across the USA demonstrates how low-tech public health measures can successfully prevent and mitigate SARS-CoV-2 transmission in outdoor programs and other group settings.
A full CDC report on this case is available at cdc.gov/mmwr/volumes/69/wr/mm6935e1.htm.
Case Study 2
But not all US outdoor programs in summer 2020 were so well-managed.
Another camp opened for the season but shut its doors only four days later; the virus had spread rapidly throughout the camp, and a stunning 76 percent of the 344 attendees for whom test results were available tested positive for the coronavirus.
The camp followed what limited guidance the state government provided, requiring staff and campers of overnight camps to provide documentation of a negative SARS-COv-2 test within the last 12 days.
The camp also:
- cohorted attendees by cabin
- staggered use of communal spaces by cohorts
- practiced physical distancing outside of cabin cohorts
- enhanced cleaning and disinfection

But contrary to CDC guidance, cloth masks were only required for staff, not campers, and doors and windows were not opened to increase ventilation indoors, where attendees regularly cheered and sang vigorously.
After being open for only four days, the camp closed for the season. The camp operator stated it regretted the decision to open the camp.
This case illustrates the importance of fully following public health agency guidance in order to prevent rampant spread of the SARS-CoV-2 virus.
Additional detail on this case is available at viristar.com/post/rapid-spread-of-coronavirus-in-summer-camp-raises-alarms.

Root Causes
As we bring this look at COVID-19 in outdoor programming to a close, let’s spend a moment with underlying risk domains, and investigate the root causes of the COVID-19 pandemic.
(Underlying risk domains have to do with government, society in general, the outdoor/ experiential industry, and the corporate/business world, and how actions of players in these domains affect risks for outdoor programs and their participants.)
We do this because we know that more pandemics will follow, and it’s better to prevent pandemics from occurring in the first place than to attempt to respond to them.
And steps to help prevent future pandemics are clear.
Pandemics exist within a complex socio-technical system, and multiple factors influence the behavior of that system:
- Public health
- Policy-making
- Health care
- Health policy
- Civic culture
- Education
- Social equity
- Institutional settings
- Media
- Environmental factors
We’ll briefly cover each one here, in turn.
Public health
Substantially increased financial and political support for public health globally can have a dramatically positive impact.
This includes measures such as rapid disease detection and response, vaccination campaigns, increasing epidemiological and public health capacity in low-income countries, and searching for viruses in nature and developing broadly effective vaccines in advance of the virus’s jump to humans, among other measures.
Policy-making
Sound policy-making based on epidemiology rather than political ideology is also essential.
Note that these and other measures are easier said than done, but we can be informed and inspired by Nordic countries and New Zealand as examples of where these root causes are relatively well-addressed.
Health care
A universally accessible, high-quality healthcare system focused on prevention rather than profit-making can mitigate pandemic effects.
Health policy
Laws and regulations promoting good health and disease-resiliency measures such as diet, exercise, strong social connections, and pollution/toxin avoidance (ranging from air quality to alcohol and tobacco) can increase disease resiliency.
Civic culture
When a society emphasizes an ethos of responsibility, collaboration, discipline and compassion, benefits accrue across many elements of society.
Education
When all individuals, regardless of socioeconomic status, sex, religion, citizenship, or other characteristics, have access to high quality pre-K through college education, they’re better-equipped to make good health decisions and advance sound health policies.
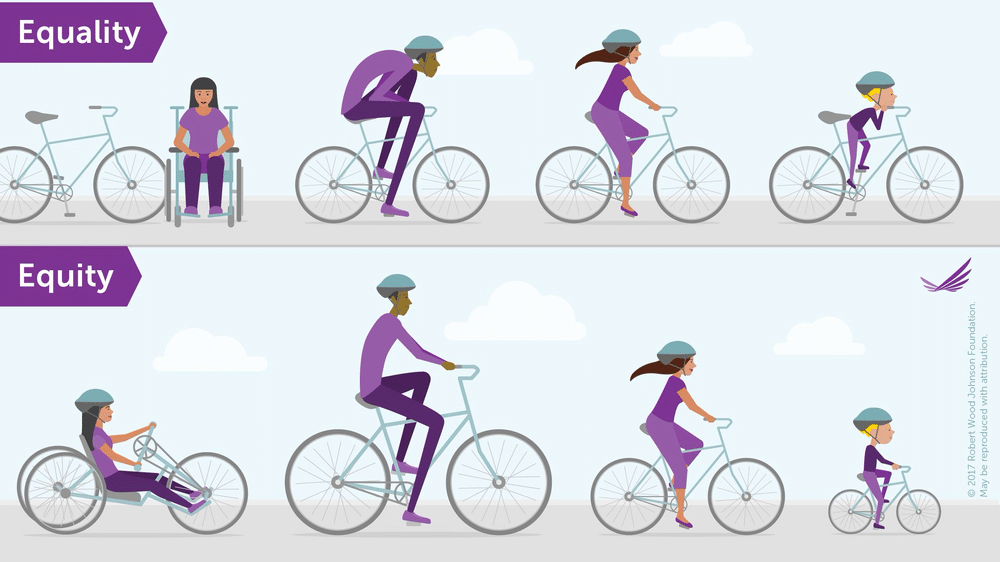
Social equity
COVID-19 has hit the world’s less privileged disproportionately hard.
Disenfranchised persons may include those not of a society’s dominant race, sex, culture, or religion, and those incarcerated or with mental illness.
Improving social equity can ease that crushing burden.
It can also reduce the probability of pandemics by, for instance, decreasing the need for some in low-income countries to seek bushmeat, which can accelerate the jump of viruses to people.
Institutional setting reform
Experts have called for improving conditions in prisons, nursing homes, and similar settings, as well as reducing prison populations, to reduce pandemic transmission.
Media and disinformation
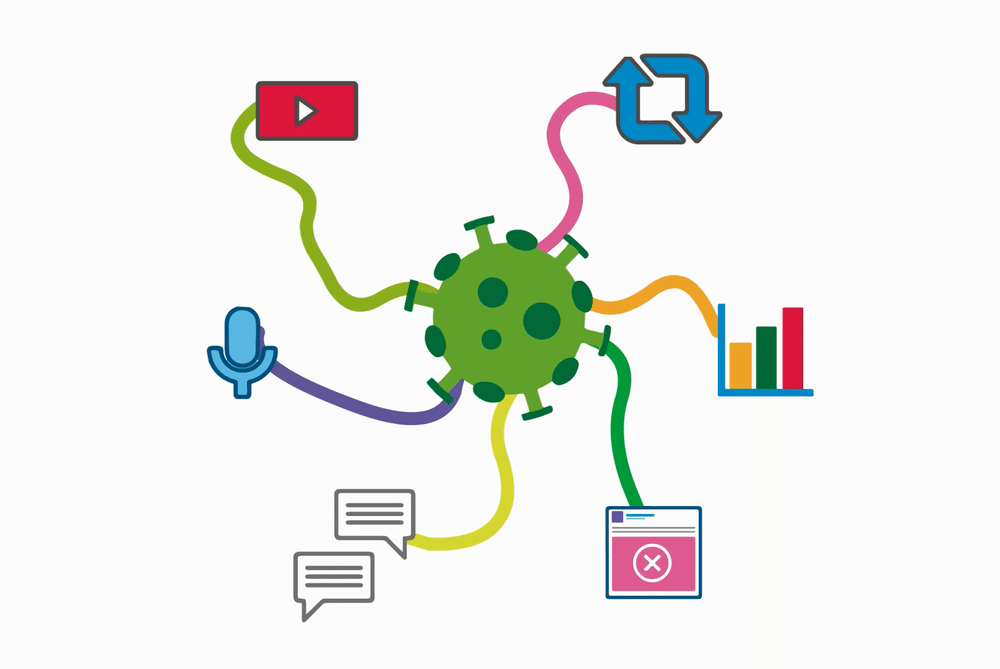
Steps to reduce or eliminate the spread of disinformation—via social media, established media, political leadership, or other vectors—can have profound positive effects.
Environmental factors
And finally, addressing a variety of environmental factors can help prevent further pandemics.
A changing climate leads animals to seek new homes, bringing viruses and humans in closer contact. Climate change leads to an increase in pandemics.
Climate change also stresses health systems, reducing care available to those who need it. And it may drive dangerous new viral mutations, among other negative effects.
The breathtakingly massive destruction of wildlife habitat currently underway—through road-building, farming, mining, deforestation, and more, including in previously remote places—along with wildlife trade for food, traditional medicines and pets, brings humans into previously wild spaces, causing increased contact with zoonotic disease vectors.

Examples of the spill-over of pathogens from a wildlife reservoir to a human host include HIV, Ebola, swine flu, and COVID-19, among others.
And loss of biodiversity leads to emergence of disease, as surviving species dominate and may pass viruses to humans, and the loss of species that control pathogen hosts increases the presence of pathogens. Simply put: biodiversity loss increases the number of deadly new pandemics.

But with good awareness of these underlying factors leading to pandemics, and the motivation and skills to address them, we’re more prepared to make a safer, better future for all.
Anticipating the Next Crisis
As outdoor programs around the world grapple with COVID-19, we can also begin thinking about the next pandemic, or other crisis, that will come our way.
Systems thinking encourages us to engineer in resiliency to the risk management systems our organizations employ, so we can weather whatever the next challenge may be.

Participants on many outdoor programs build resilience, as they work as a team to overcome obstacles and meet their goals.
Well-prepared outdoor programs, too, can have confidence that they also, in the face of challenge, can—and will—persevere.



